Do Fallen Arches Need To Have Surgery?
Overview

?Pes Planus? is the medical term for flat feet. It comes from Latin: Pes = foot and Planus = plain, level ground. Very few people suffer from this condition, as a true flat foot is very rare. Less than 5% of the population has flat feet. The majority of the Australian population, however, has fallen arches (an estimated 60-70% of the population) known in the medical profession as ?excess pronation? or over-pronation. Over-pronation means the foot and ankle tend to roll inwards and the arch collapses with weight-bearing. This is a quite a destructive position for the foot to function in and may cause a wide variety of foot, leg and lower back conditions.
Causes
There are many different causes of flat feet, which can be separated into two main categories. The first category, congenital flat foot, is a condition that one is born with or is predisposed to at birth. This type includes the completely asymptomatic, pediatric flexible flat foot-by far the most common form of congenital flat foot. Flexible means that an arch is present until weight is put on the foot, at which time the arch disappears. This foot type is a result of the fact that all people are born with different physical features. Some people have bigger noses than others, just as some people have flatter feet (of course, there is no known correlation between the two). Any alteration in the many building blocks of the foot can influence its shape. At the other end of the spectrum, yet within the same category of congenital flat foot, exist several rare, more severe forms of flat foot. These severe conditions include Vertical Talus, Congenital Calcaneal Valgus, and Tarsal Coalitions - all of which are more rigid (no arch with or without weight on the foot) and definitely symptomatic. Luckily, these are much less common, but can usually be identified by specialists at the time of presentation and treated appropriately. The second category, acquired flat foot, develops over time, rather than at birth. Many different factors can contribute to the development of flat feet. These include the types of shoes a child wears, a child's sitting or sleeping positions, compensation for other abnormalities further up the leg, or more severe factors such as rupture of ligaments or tendons in the foot. Very commonly, the reason for flat feet is that the foot is compensating for a tight Achilles tendon. If the Achilles tendon is tight, then it causes the foot to point down, or to plantarflex (as occurs when stepping on the accelerator of your car). Even minimal amounts of plantarflexion can simulate a longer leg on that particular side, assuming that the other foot is in the normal position. The body therefore tries to compensate by pronating, or flattening out the arch, thereby making up for the perceived extra length on the affected side.
Symptoms
Fallen arches symptoms may include the following. Being unable to slip fingers underneath arches. Inwards rolling of foot and ankle when running. Knee problems due to lack of support from feet.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
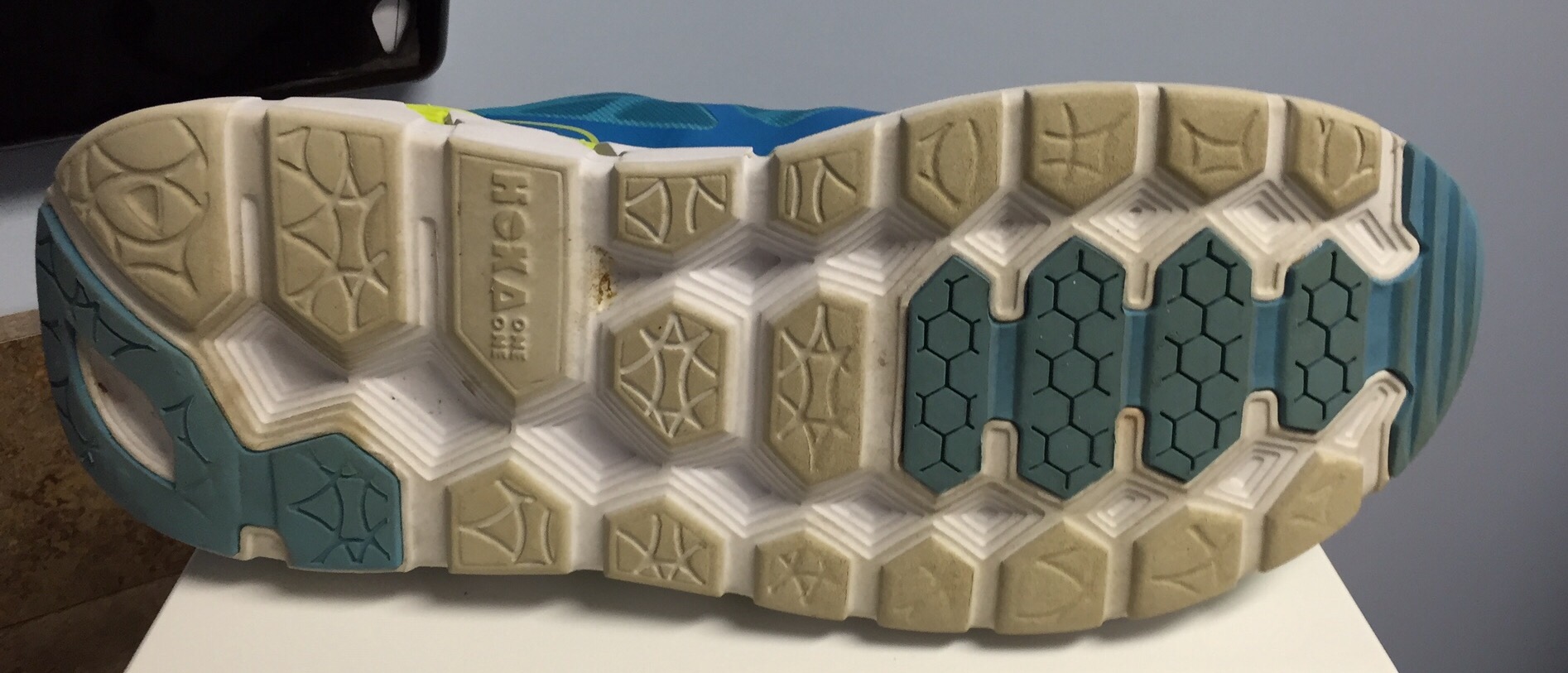
arch support plantar fasciitis
Non Surgical Treatment
Most cases of flatfeet do not require treatment. However, if there is pain, or if the condition is caused by something other than normal development, there are several treatment options. Self-care options include rest, choosing non-weight-bearing exercise (e.g., swimming, cycling), weight loss, and avoiding high heels. Flexible flatfeet with some pain can be relieved with the use of orthotics-shoe inserts that support the arch-and/or heel wedges (in some cases). If pronation is a factor, special shoes can be worn that lift the arch and correct the inward leaning. Physical therapy may also be prescribed to stretch or lengthen the heel cord and other tendons. For rigid or inflexible flatfeet, treatment varies depending on the cause. Tarsal coalition if often treated with rest and the wearing of a cast. If this is ineffective, surgery can be done to separate the bones or to reset the bones into a correct position. If the flatfoot is caused by an injury to the tendons in the foot or ankle, rest, anti-inflammatory medications (e.g., ibuprofen), and the use of shoe inserts and ankle braces often relieve symptoms. In severe cases, surgery is performed to repair the tendon or to fuse some joints in the foot into a corrected position to reduce stress on the tendon. The prognosis after surgery is generally good. Complications include pain and some loss of ankle motion, especially when trying to turn the foot in or out. This may be improved with physical therapy.
Surgical Treatment

Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch.

?Pes Planus? is the medical term for flat feet. It comes from Latin: Pes = foot and Planus = plain, level ground. Very few people suffer from this condition, as a true flat foot is very rare. Less than 5% of the population has flat feet. The majority of the Australian population, however, has fallen arches (an estimated 60-70% of the population) known in the medical profession as ?excess pronation? or over-pronation. Over-pronation means the foot and ankle tend to roll inwards and the arch collapses with weight-bearing. This is a quite a destructive position for the foot to function in and may cause a wide variety of foot, leg and lower back conditions.
Causes
There are many different causes of flat feet, which can be separated into two main categories. The first category, congenital flat foot, is a condition that one is born with or is predisposed to at birth. This type includes the completely asymptomatic, pediatric flexible flat foot-by far the most common form of congenital flat foot. Flexible means that an arch is present until weight is put on the foot, at which time the arch disappears. This foot type is a result of the fact that all people are born with different physical features. Some people have bigger noses than others, just as some people have flatter feet (of course, there is no known correlation between the two). Any alteration in the many building blocks of the foot can influence its shape. At the other end of the spectrum, yet within the same category of congenital flat foot, exist several rare, more severe forms of flat foot. These severe conditions include Vertical Talus, Congenital Calcaneal Valgus, and Tarsal Coalitions - all of which are more rigid (no arch with or without weight on the foot) and definitely symptomatic. Luckily, these are much less common, but can usually be identified by specialists at the time of presentation and treated appropriately. The second category, acquired flat foot, develops over time, rather than at birth. Many different factors can contribute to the development of flat feet. These include the types of shoes a child wears, a child's sitting or sleeping positions, compensation for other abnormalities further up the leg, or more severe factors such as rupture of ligaments or tendons in the foot. Very commonly, the reason for flat feet is that the foot is compensating for a tight Achilles tendon. If the Achilles tendon is tight, then it causes the foot to point down, or to plantarflex (as occurs when stepping on the accelerator of your car). Even minimal amounts of plantarflexion can simulate a longer leg on that particular side, assuming that the other foot is in the normal position. The body therefore tries to compensate by pronating, or flattening out the arch, thereby making up for the perceived extra length on the affected side.
Symptoms
Fallen arches symptoms may include the following. Being unable to slip fingers underneath arches. Inwards rolling of foot and ankle when running. Knee problems due to lack of support from feet.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
arch support plantar fasciitis
Non Surgical Treatment
Most cases of flatfeet do not require treatment. However, if there is pain, or if the condition is caused by something other than normal development, there are several treatment options. Self-care options include rest, choosing non-weight-bearing exercise (e.g., swimming, cycling), weight loss, and avoiding high heels. Flexible flatfeet with some pain can be relieved with the use of orthotics-shoe inserts that support the arch-and/or heel wedges (in some cases). If pronation is a factor, special shoes can be worn that lift the arch and correct the inward leaning. Physical therapy may also be prescribed to stretch or lengthen the heel cord and other tendons. For rigid or inflexible flatfeet, treatment varies depending on the cause. Tarsal coalition if often treated with rest and the wearing of a cast. If this is ineffective, surgery can be done to separate the bones or to reset the bones into a correct position. If the flatfoot is caused by an injury to the tendons in the foot or ankle, rest, anti-inflammatory medications (e.g., ibuprofen), and the use of shoe inserts and ankle braces often relieve symptoms. In severe cases, surgery is performed to repair the tendon or to fuse some joints in the foot into a corrected position to reduce stress on the tendon. The prognosis after surgery is generally good. Complications include pain and some loss of ankle motion, especially when trying to turn the foot in or out. This may be improved with physical therapy.
Surgical Treatment

Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch.
Leg Length Discrepancy Gait
Overview
Differences between lengths of the two upper extremities (upper and/or lower arms) or between the lengths of the two lower extremities (upper and/or lower legs) are called limb length discrepancy (LLD). A limb length discrepancy may be due to a normal variation that we all have between the two sides of our bodies, or it may be due to other causes. Some differences are so common that they are normal and need no treatment. For example, one study reported that 32 percent of 600 military recruits had a 5mm to 15mm (approximately 1/5 to 3/5 inch) difference between the lengths of their two lower extremities; this is a normal variation. Greater differences may need treatment because a discrepancy can affect a patient?s well being and quality of life.
Causes
Some children are born with absence or underdeveloped bones in the lower limbs e.g., congenital hemimelia. Others have a condition called hemihypertrophy that causes one side of the body to grow faster than the other. Sometimes, increased blood flow to one limb (as in a hemangioma or blood vessel tumor) stimulates growth to the limb. In other cases, injury or infection involving the epiphyseal plate (growth plate) of the femur or tibia inhibits or stops altogether the growth of the bone. Fractures healing in an overlapped position, even if the epiphyseal plate is not involved, can also cause limb length discrepancy. Neuromuscular problems like polio can also cause profound discrepancies, but thankfully, uncommon. Lastly, Wilms? tumor of the kidney in a child can cause hypertrophy of the lower limb on the same side. It is therefore important in a young child with hemihypertrophy to have an abdominal ultrasound exam done to rule out Wilms? tumor. It is important to distinguish true leg length discrepancy from apparent leg length discrepancy. Apparent discrepancy is due to an instability of the hip, that allows the proximal femur to migrate proximally, or due to an adduction or abduction contracture of the hip that causes pelvic obliquity, so that one hip is higher than the other. When the patient stands, it gives the impression of leg length discrepancy, when the problem is actually in the hip.
Symptoms
Faulty feet and ankle structure profoundly affect leg length and pelvic positioning. The most common asymmetrical foot position is the pronated foot. Sensory receptors embedded on the bottom of the foot alert the brain to the slightest weight shift. Since the brain is always trying to maintain pelvic balance, when presented with a long left leg, it attempts to adapt to the altered weight shift by dropping the left medial arch (shortening the long leg) and supinating the right arch to lengthen the short leg.1 Left unchecked, excessive foot pronation will internally rotate the left lower extremity, causing excessive strain to the lateral meniscus and medial collateral knee ligaments. Conversely, excessive supination tends to externally rotate the leg and thigh, creating opposite knee, hip and pelvic distortions.
Diagnosis
On standing examination one iliac crest may be higher/lower than the other. However a physiotherapist, osteopath or chiropractor will examine the LLD in prone or supine position and measure it, confirming the diagnosis of structural (or functional) LLD. The LLD should be measured using bony fixed points. X-Ray should be taken in a standing position. The osteopath, physiotherapist or chiropractor will look at femoral head & acetabulum, knee joints, ankle joints.
Non Surgical Treatment
The way in which we would treat a LLD would depend on whether we have an anatomical or functional difference. To determine which one is causing the LLD you will need to get your legs measured. This is the easiest way to determine if it is anatomical or functional. With a functional LLD we must first determine the cause and treat the cause. Should the cause be one that is not correctable then we may need to treat the LLD as if it were an anatomical or may have to treat the opposite leg to improve one's gait. As for the anatomical LLD, we may start off with a heel lift only in the shoe and follow up to see if we will need to put the lift full sole on the bottom of the shoe. This is determined by the affects that a heel lift in one shoe may have on that knee. Should the LLD be more than 1/4 inch we usually recommend starting between 1/8 inch to 1/4 inch less than the actual amount and let the body adjust to the change and then raise up to the measured amount later.

what is a shoe lift?
Surgical Treatment
Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces.
Differences between lengths of the two upper extremities (upper and/or lower arms) or between the lengths of the two lower extremities (upper and/or lower legs) are called limb length discrepancy (LLD). A limb length discrepancy may be due to a normal variation that we all have between the two sides of our bodies, or it may be due to other causes. Some differences are so common that they are normal and need no treatment. For example, one study reported that 32 percent of 600 military recruits had a 5mm to 15mm (approximately 1/5 to 3/5 inch) difference between the lengths of their two lower extremities; this is a normal variation. Greater differences may need treatment because a discrepancy can affect a patient?s well being and quality of life.

Causes
Some children are born with absence or underdeveloped bones in the lower limbs e.g., congenital hemimelia. Others have a condition called hemihypertrophy that causes one side of the body to grow faster than the other. Sometimes, increased blood flow to one limb (as in a hemangioma or blood vessel tumor) stimulates growth to the limb. In other cases, injury or infection involving the epiphyseal plate (growth plate) of the femur or tibia inhibits or stops altogether the growth of the bone. Fractures healing in an overlapped position, even if the epiphyseal plate is not involved, can also cause limb length discrepancy. Neuromuscular problems like polio can also cause profound discrepancies, but thankfully, uncommon. Lastly, Wilms? tumor of the kidney in a child can cause hypertrophy of the lower limb on the same side. It is therefore important in a young child with hemihypertrophy to have an abdominal ultrasound exam done to rule out Wilms? tumor. It is important to distinguish true leg length discrepancy from apparent leg length discrepancy. Apparent discrepancy is due to an instability of the hip, that allows the proximal femur to migrate proximally, or due to an adduction or abduction contracture of the hip that causes pelvic obliquity, so that one hip is higher than the other. When the patient stands, it gives the impression of leg length discrepancy, when the problem is actually in the hip.
Symptoms
Faulty feet and ankle structure profoundly affect leg length and pelvic positioning. The most common asymmetrical foot position is the pronated foot. Sensory receptors embedded on the bottom of the foot alert the brain to the slightest weight shift. Since the brain is always trying to maintain pelvic balance, when presented with a long left leg, it attempts to adapt to the altered weight shift by dropping the left medial arch (shortening the long leg) and supinating the right arch to lengthen the short leg.1 Left unchecked, excessive foot pronation will internally rotate the left lower extremity, causing excessive strain to the lateral meniscus and medial collateral knee ligaments. Conversely, excessive supination tends to externally rotate the leg and thigh, creating opposite knee, hip and pelvic distortions.
Diagnosis
On standing examination one iliac crest may be higher/lower than the other. However a physiotherapist, osteopath or chiropractor will examine the LLD in prone or supine position and measure it, confirming the diagnosis of structural (or functional) LLD. The LLD should be measured using bony fixed points. X-Ray should be taken in a standing position. The osteopath, physiotherapist or chiropractor will look at femoral head & acetabulum, knee joints, ankle joints.
Non Surgical Treatment
The way in which we would treat a LLD would depend on whether we have an anatomical or functional difference. To determine which one is causing the LLD you will need to get your legs measured. This is the easiest way to determine if it is anatomical or functional. With a functional LLD we must first determine the cause and treat the cause. Should the cause be one that is not correctable then we may need to treat the LLD as if it were an anatomical or may have to treat the opposite leg to improve one's gait. As for the anatomical LLD, we may start off with a heel lift only in the shoe and follow up to see if we will need to put the lift full sole on the bottom of the shoe. This is determined by the affects that a heel lift in one shoe may have on that knee. Should the LLD be more than 1/4 inch we usually recommend starting between 1/8 inch to 1/4 inch less than the actual amount and let the body adjust to the change and then raise up to the measured amount later.

what is a shoe lift?
Surgical Treatment
Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces.
Understand Heel Discomfort
Overview

Heel pain is a common foot condition. It's usually felt as an intense pain when using the affected heel. Heel pain usually builds up gradually and gets worse over time. The pain is often severe and occurs when you place weight on the heel. In most cases, only one heel is affected, although estimates suggest that around a third of people have pain in both heels. The pain is usually worse first thing in the morning, or when you first take a step after a period of inactivity. Walking usually improves the pain, but it often gets worse again after walking or standing for a long time. Some people may limp or develop an abnormal walking style as they try to avoid placing weight on the affected heel.
Causes
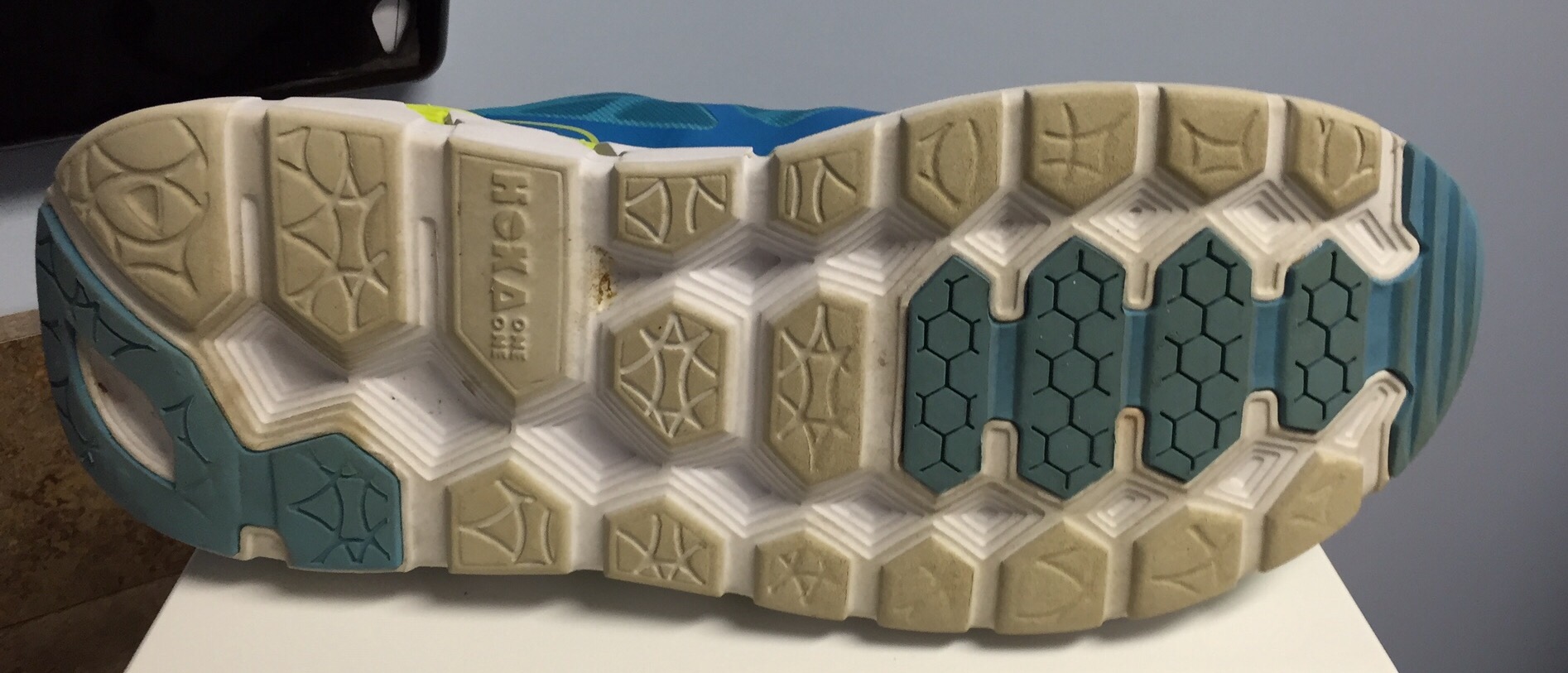
The most common cause of heel pain in adults is plantar fasciitis, which is an inflammation of the band of tissue in the sole that connects the heel to the toes and forms the natural foot arch. Plantar fasciitis may or may not be complicated by a calcaneal spur, a small bone growth that protrudes out of the heel. Plantar fasciitis may also be referred to as plantar fasciosis. In contrast to fasciitis, which essentially means inflammation, fasciosis refers to degeneration of the tissue. In fact, if left untreated, acute plantar fasciitis may develop into a chronic painful condition, which results in slow and irreversible degeneration of the fascia, hence plantar fasciosis. The location of the pain is usually exactly under the heel but may also occur in the arch of the foot. Pain typical to plantar fasciitis is that which feels worse when arising on to your feet such as in mornings or after sitting down for a while, and usually progresses in severity when left untreated.
Symptoms
The primary symptom is pain in the heel area that varies in severity and location. The pain is commonly intense when getting out of bed or a chair. The pain often lessens when walking.
Diagnosis
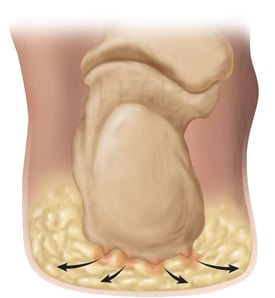
Your doctor will listen to your complaints about your heel and examine you to see what is causing the pain, and whether anything else has started it off. If the cause of your pain seems obvious, your doctor may be happy to start treatment straight away. However, some tests may be helpful in ruling out other problems. Blood tests may be done for arthritis. An Xray will show any arthritis in the ankle or subtalar joint, as well as any fracture or cyst in the calcaneum. (It will also show a spur if you have one, but as we know this is not the cause of the pain.) Occasionally a scan may be used to help spot arthritis or a stress fracture.
Non Surgical Treatment
Early treatment might involve exercise and shoe recommendations, taping or strapping and anti-inflammatory medication (such as aspirin). Taping or strapping supports the foot, placing stressed muscles in a restful state and preventing stretching of the plantar fascia. Other physical therapies may also be used, including ice packs and ultra-sounds. These treatments will effectively treat the majority of heel and arch pain without the need for surgery.
Surgical Treatment
Extracorporeal shockwave therapy (EST) is a fairly new type of non-invasive treatment. Non-invasive means it does not involve making cuts into your body. EST involves using a device to deliver high-energy soundwaves into your heel. The soundwaves can sometimes cause pain, so a local anaesthetic may be used to numb your heel. It is claimed that EST works in two ways. It is thought to have a "numbing" effect on the nerves that transmit pain signals to your brain, help stimulate and speed up the healing process. However, these claims have not yet been definitively proven. The National Institute for Health and Care Excellence (NICE) has issued guidance about the use of EST for treating plantar fasciitis. NICE states there are no concerns over the safety of EST, but there are uncertainties about how effective the procedure is for treating heel pain. Some studies have reported that EST is more effective than surgery and other non-surgical treatments, while other studies found the procedure to be no better than a placebo (sham treatment).
bestshoelifts
Prevention

Wearing real good, supportive shoes are a great way to avoid heel pain. Usually, New Balance is a good shoe to wear, just for everyday shoe gear. By wearing proper footwear and performing thorough stretches, athletes can help prevent frequent heel pain. If you are starting to get a little discomfort or pain in the feet or heel, know that pain is not normal. So if you are having pain, you should be proactive and visit our office. If you let heel pain get out of control you could run into several other problems. It is always suggested to visit a podiatrist whenever you are experiencing pain.

Heel pain is a common foot condition. It's usually felt as an intense pain when using the affected heel. Heel pain usually builds up gradually and gets worse over time. The pain is often severe and occurs when you place weight on the heel. In most cases, only one heel is affected, although estimates suggest that around a third of people have pain in both heels. The pain is usually worse first thing in the morning, or when you first take a step after a period of inactivity. Walking usually improves the pain, but it often gets worse again after walking or standing for a long time. Some people may limp or develop an abnormal walking style as they try to avoid placing weight on the affected heel.
Causes
The most common cause of heel pain in adults is plantar fasciitis, which is an inflammation of the band of tissue in the sole that connects the heel to the toes and forms the natural foot arch. Plantar fasciitis may or may not be complicated by a calcaneal spur, a small bone growth that protrudes out of the heel. Plantar fasciitis may also be referred to as plantar fasciosis. In contrast to fasciitis, which essentially means inflammation, fasciosis refers to degeneration of the tissue. In fact, if left untreated, acute plantar fasciitis may develop into a chronic painful condition, which results in slow and irreversible degeneration of the fascia, hence plantar fasciosis. The location of the pain is usually exactly under the heel but may also occur in the arch of the foot. Pain typical to plantar fasciitis is that which feels worse when arising on to your feet such as in mornings or after sitting down for a while, and usually progresses in severity when left untreated.
Symptoms
The primary symptom is pain in the heel area that varies in severity and location. The pain is commonly intense when getting out of bed or a chair. The pain often lessens when walking.
Diagnosis
Your doctor will listen to your complaints about your heel and examine you to see what is causing the pain, and whether anything else has started it off. If the cause of your pain seems obvious, your doctor may be happy to start treatment straight away. However, some tests may be helpful in ruling out other problems. Blood tests may be done for arthritis. An Xray will show any arthritis in the ankle or subtalar joint, as well as any fracture or cyst in the calcaneum. (It will also show a spur if you have one, but as we know this is not the cause of the pain.) Occasionally a scan may be used to help spot arthritis or a stress fracture.
Non Surgical Treatment
Early treatment might involve exercise and shoe recommendations, taping or strapping and anti-inflammatory medication (such as aspirin). Taping or strapping supports the foot, placing stressed muscles in a restful state and preventing stretching of the plantar fascia. Other physical therapies may also be used, including ice packs and ultra-sounds. These treatments will effectively treat the majority of heel and arch pain without the need for surgery.
Surgical Treatment
Extracorporeal shockwave therapy (EST) is a fairly new type of non-invasive treatment. Non-invasive means it does not involve making cuts into your body. EST involves using a device to deliver high-energy soundwaves into your heel. The soundwaves can sometimes cause pain, so a local anaesthetic may be used to numb your heel. It is claimed that EST works in two ways. It is thought to have a "numbing" effect on the nerves that transmit pain signals to your brain, help stimulate and speed up the healing process. However, these claims have not yet been definitively proven. The National Institute for Health and Care Excellence (NICE) has issued guidance about the use of EST for treating plantar fasciitis. NICE states there are no concerns over the safety of EST, but there are uncertainties about how effective the procedure is for treating heel pain. Some studies have reported that EST is more effective than surgery and other non-surgical treatments, while other studies found the procedure to be no better than a placebo (sham treatment).
bestshoelifts
Prevention

Wearing real good, supportive shoes are a great way to avoid heel pain. Usually, New Balance is a good shoe to wear, just for everyday shoe gear. By wearing proper footwear and performing thorough stretches, athletes can help prevent frequent heel pain. If you are starting to get a little discomfort or pain in the feet or heel, know that pain is not normal. So if you are having pain, you should be proactive and visit our office. If you let heel pain get out of control you could run into several other problems. It is always suggested to visit a podiatrist whenever you are experiencing pain.
Mortons Neuroma Solutions
Overview
 If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. Morton's neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.
If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. Morton's neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.
Causes
Various factors have been implicated in the precipitation of Morton's neuroma. Morton's neuroma is known to develop as a result of chronic nerve stress and irritation, particularly with excessive toe dorsiflexion. Poorly fitting and constricting shoes (ie, small toe box) or shoes with heel lifts often contribute to Morton's neuroma. Women who wear high-heeled shoes for a number of years or men who are required to wear constrictive shoe gear are at risk. A biomechanical theory of causation involves the mechanics of the foot and ankle. For instance, individuals with tight gastrocnemius-soleus muscles or who excessively pronate the foot may compensate by dorsiflexion of the metatarsals subsequently irritating of the interdigital nerve. Certain activities carry increased risk of excessive toe dorsiflexion, such as prolonged walking, running, squatting, and demi-pointe position in ballet.
Symptoms
Symptoms of interdigital neuroma typically manifest as a sharp, burning or tingling sensation in the forefoot. The pain radiates toward the lesser toes and is aggravated by shoe wear. The pain is relieved when the shoe is removed and the forefoot is massaged. Sometimes the symptoms involve specific toes.
Diagnosis
To arrive at a diagnosis, the foot and ankle surgeon will obtain a thorough history of your symptoms and examine your foot. During the physical examination, the doctor attempts to reproduce your symptoms by manipulating your foot. Other tests or imaging studies may be performed. The best time to see your foot and ankle surgeon is early in the development of symptoms. Early diagnosis of a Morton?s neuroma greatly lessens the need for more invasive treatments and may avoid surgery.
Non Surgical Treatment
Treatments may include rehabilitation measures to reduce nerve Irritation. Switching to low-heeled, wide-toed shoes with good arch support. Wearing padding in the shoes and/or between the toes. Wearing shoe inserts to correct a mechanical abnormality of the foot. Having ultrasound, electrical stimulation, whirlpool, and massage done on the foot. The foot may be injected with corticosteroids mixed with a local anesthetic in order to reduce pain. Relief may be only temporary, however, if the mechanical irritation is not also corrected. Injections with other types of medications such as alcohol, phenol, or vitamin B12 are sometimes used.
Surgical Treatment
Majority of publications including peer review journal articles, surgical technique description and textbooks promote surgical excision as a gold standard treatment. Surgical excision is described as the most definitive mode of treatment for symptomatic Morton?s neuroma with reported success rates varying between 79% and 93%. Various surgical techniques are described, essentially categorised as dorsal versus plantar incision approaches. Beyond this the commonest technical variation described as influencing the outcome of surgery involves burying and anchoring transacted nerve into soft tissue such as muscle.
Prevention
Wearing proper footwear that minimizes compression of the forefoot can help to prevent the development of and aggravation of a Morton's neuroma.
 If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. Morton's neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.
If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. Morton's neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.Causes
Various factors have been implicated in the precipitation of Morton's neuroma. Morton's neuroma is known to develop as a result of chronic nerve stress and irritation, particularly with excessive toe dorsiflexion. Poorly fitting and constricting shoes (ie, small toe box) or shoes with heel lifts often contribute to Morton's neuroma. Women who wear high-heeled shoes for a number of years or men who are required to wear constrictive shoe gear are at risk. A biomechanical theory of causation involves the mechanics of the foot and ankle. For instance, individuals with tight gastrocnemius-soleus muscles or who excessively pronate the foot may compensate by dorsiflexion of the metatarsals subsequently irritating of the interdigital nerve. Certain activities carry increased risk of excessive toe dorsiflexion, such as prolonged walking, running, squatting, and demi-pointe position in ballet.
Symptoms
Symptoms of interdigital neuroma typically manifest as a sharp, burning or tingling sensation in the forefoot. The pain radiates toward the lesser toes and is aggravated by shoe wear. The pain is relieved when the shoe is removed and the forefoot is massaged. Sometimes the symptoms involve specific toes.
Diagnosis
To arrive at a diagnosis, the foot and ankle surgeon will obtain a thorough history of your symptoms and examine your foot. During the physical examination, the doctor attempts to reproduce your symptoms by manipulating your foot. Other tests or imaging studies may be performed. The best time to see your foot and ankle surgeon is early in the development of symptoms. Early diagnosis of a Morton?s neuroma greatly lessens the need for more invasive treatments and may avoid surgery.
Non Surgical Treatment
Treatments may include rehabilitation measures to reduce nerve Irritation. Switching to low-heeled, wide-toed shoes with good arch support. Wearing padding in the shoes and/or between the toes. Wearing shoe inserts to correct a mechanical abnormality of the foot. Having ultrasound, electrical stimulation, whirlpool, and massage done on the foot. The foot may be injected with corticosteroids mixed with a local anesthetic in order to reduce pain. Relief may be only temporary, however, if the mechanical irritation is not also corrected. Injections with other types of medications such as alcohol, phenol, or vitamin B12 are sometimes used.

Surgical Treatment
Majority of publications including peer review journal articles, surgical technique description and textbooks promote surgical excision as a gold standard treatment. Surgical excision is described as the most definitive mode of treatment for symptomatic Morton?s neuroma with reported success rates varying between 79% and 93%. Various surgical techniques are described, essentially categorised as dorsal versus plantar incision approaches. Beyond this the commonest technical variation described as influencing the outcome of surgery involves burying and anchoring transacted nerve into soft tissue such as muscle.
Prevention
Wearing proper footwear that minimizes compression of the forefoot can help to prevent the development of and aggravation of a Morton's neuroma.
How Shoe Lifts Overcome Leg Length Discrepancy
There are actually not one but two unique variations of leg length discrepancies, congenital and acquired. Congenital indicates you are born with it. One leg is structurally shorter compared to the other. Through developmental periods of aging, the brain picks up on the gait pattern and identifies some variation. The entire body typically adapts by dipping one shoulder to the "short" side. A difference of under a quarter inch isn't grossly excessive, demand Shoe Lifts to compensate and normally won't have a serious effect over a lifetime.

Leg length inequality goes typically undiscovered on a daily basis, yet this condition is simply corrected, and can eradicate a number of cases of back ache.
Treatment for leg length inequality commonly involves Shoe Lifts. They are low cost, typically costing below twenty dollars, in comparison to a custom orthotic of $200 plus. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Upper back pain is easily the most widespread condition impacting people today. Over 80 million people are affected by back pain at some stage in their life. It is a problem which costs employers millions of dollars yearly because of lost time and production. Fresh and superior treatment solutions are constantly sought after in the hope of reducing the economic impact this issue causes.

People from all corners of the world experience foot ache as a result of leg length discrepancy. In these situations Shoe Lifts might be of worthwhile. The lifts are capable of reducing any pain in the feet. Shoe Lifts are recommended by countless experienced orthopaedic practitioners".
To be able to support the body in a well-balanced manner, your feet have a very important part to play. Despite that, it can be the most overlooked area of the human body. Some people have flat-feet meaning there may be unequal force placed on the feet. This causes other body parts such as knees, ankles and backs to be affected too. Shoe Lifts make sure that the right posture and balance are restored.

Leg length inequality goes typically undiscovered on a daily basis, yet this condition is simply corrected, and can eradicate a number of cases of back ache.
Treatment for leg length inequality commonly involves Shoe Lifts. They are low cost, typically costing below twenty dollars, in comparison to a custom orthotic of $200 plus. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Upper back pain is easily the most widespread condition impacting people today. Over 80 million people are affected by back pain at some stage in their life. It is a problem which costs employers millions of dollars yearly because of lost time and production. Fresh and superior treatment solutions are constantly sought after in the hope of reducing the economic impact this issue causes.

People from all corners of the world experience foot ache as a result of leg length discrepancy. In these situations Shoe Lifts might be of worthwhile. The lifts are capable of reducing any pain in the feet. Shoe Lifts are recommended by countless experienced orthopaedic practitioners".
To be able to support the body in a well-balanced manner, your feet have a very important part to play. Despite that, it can be the most overlooked area of the human body. Some people have flat-feet meaning there may be unequal force placed on the feet. This causes other body parts such as knees, ankles and backs to be affected too. Shoe Lifts make sure that the right posture and balance are restored.
Do I Have Posterior Calcaneal Spur

Overview
There are approximately 75 different causes of heel pain. At least 80% of all heel pain is due to heel spurs. A heel spur contains calcium, but cannot truly be called a calcium deposit. Bone spurs, whether they are on the heel or on any other bone of the body, are true bone -- they are true enlargements of the bone and may be sharp and pointed, or round and knobby. Since bone spurs are true bone, they contain calcium just like regular bones, but are not pure calcium deposits.
Causes
A heel spur is a bony overgrowth on the bottom of your heel bone. The heel spur is usually a result of an inflamed ligament (plantar fascia) on the bottom of the foot that attaches to the heel bone. Constant abnormal pulling of this ligament irritates the heel bone and the body lays down a bone spur as a protective mechanism. The patient usually complains of pain with the first step in the morning, some relief following activity, but returning after extended amounts of time standing or walking.

Symptoms
You may or may not experience any symptoms with your heel spurs. It is normally the irritation and inflammation felt in the tissues around your heel spur that cause discomfort. Heel pain is one of the first things you may notice, especially when pushing off the ball of your foot (stretches the plantar fascia). The pain can get worse over time and tends to be stronger in the morning, subsiding throughout the day; although it does return with increased activity. A sharp, poking pain in your heel that feels like you're stepping on a stone can often be felt while standing or walking. You will sometimes be able to feel a bump on the bottom of your heel, and occasionally bruising may appear.
Diagnosis
Heel spurs and plantar fasciitis are diagnosed based on the history of pain and tenderness localized to these areas. They are specifically identified when there is point tenderness at the bottom of the heel, which makes it difficult to walk barefoot on tile or wood floors. X-ray examination of the foot is used to identify the bony prominence (spur) of the heel bone (calcaneus).
Non Surgical Treatment
Elevation of the affected foot and leg at rest may diminish the pain. Applying gentle heat to the painful area may ease the pain by dilating local blood vessels. One also can protect the heel by placing a foam rubber pad in the heel of the shoe. A pad about one-half inch thick will raise the heel, shift the weight of the body forward, and protect the irritated muscles attached to the heel bone. The same effect can be achieved by using adhesive tape to turn the foot inward. Additional treatment may consist of a number of physical therapies, such as diathermy, ultrasound waves and whirlpool baths.
Surgical Treatment
Usually, heel spurs are curable with conservative treatment. If not, heel spurs are curable with surgery, although there is the possibility of them growing back. About 10% of those who continue to see a physician for plantar fascitis have it for more than a year. If there is limited success after approximately one year of conservative treatment, patients are often advised to have surgery.
Inferior Calcaneal Spur Symtoms
Overview
Bone spurs usually form around joints that have arthritis, in the vertebrae of the spine, and on the heel. When they form on the heel, they may form on the back of the heel but usually form on the bottom of the heel. Of course, this is where all of the body weight comes down with each step. Spurs on the bottom of the heel are usually most painful the first few steps out of bed each morning. The pain may lessen somewhat after walking for a few minutes, but may be intense again after sitting for a half hour or so, such as after lunch. The pain usually gets worse throughout the day as you are up on your feet more. Often the pain feels like a nail being driven through the heel into the ankle and leg.
Causes
Diseases such as arthritis may lead to chronic inflammation in the tissue surrounding the heel and over time this can lead to the accumulation of calcium deposits. Ankylosing spondylitis, for example, is one particular form of arthritis that frequently develops along with heel spurs. This condition can damage bones all over the body and even lead to the fusion of spinal vertebrae.
Symptoms
Heel spurs can be quite painful, but can just as likely occur with no symptoms at all. Plantar fasciitis is a contributing condition to heel spurs. The cause of the pain is not the heel spur itself but the soft-tissue injury associated with it. The feeling has been described as a knife or pin sticking into the bottom of your feet when you first stand up after sitting or laying down for a long period of time - a pain that later turns into a dull ache.
Diagnosis
A thorough medical history and physical exam by a physician is always necessary for the proper diagnosis of heel spurs and other foot conditions. X rays of the heel area are helpful, as excess bone production will be visible.
Non Surgical Treatment
In some cases, heel spur pain may not be resolved through conservative treatment options. In those cases, cortisone injections may be used to reduce inflammation associated with the condition, helping to reduce discomfort. However, treatment options such as these must be discussed in detail with your physician, since more serious forms of treatment could yield negative side effects, such as atrophy of the heel's fat pad, or the rupture of the plantar fascia ligament. Although such side effects are rare, they are potential problems that could deliver added heel pain.
Surgical Treatment
Usually, heel spurs are curable with conservative treatment. If not, heel spurs are curable with surgery, although there is the possibility of them growing back. About 10% of those who continue to see a physician for plantar fascitis have it for more than a year. If there is limited success after approximately one year of conservative treatment, patients are often advised to have surgery.
Prevention
A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don't underestimate your body's need for rest and good nutrition. If obese, lose weight.